Find out why Guided Biofilm Therapy (GBT) is a more effective yet gentle alternative approach to removing biofilm that restores oral microbiome balance, promotes patient education, and how it actually works in practice.
Why GBT?
You may be asking yourself, why do I need another tool in my dental operatory? We have been providing professional dental therapy for decades, so why do we need to change what we are doing? As dental hygienists we need to embrace change to adapt to the knowledge that we have available to us. We now know that biofilm is the root cause of disease and inflammation in our mouths. Our traditional methods of preventative and non-surgical periodontal therapy have been appropriate in the past, and we have done the best we could with what was made available to us. However, we need to adapt to the evolution of dental hygiene with our patients comfort and compliance in mind. Guided Biofilm Therapy (GBT) gives us the opportunity to remove biofilm more adequately and less invasively and be highly effective and efficient. As a dental hygienist, I am motivated to follow the 8-step protocol of Guided Biofilm Therapy, which allows me to have difficult conversations with my patients about their oral health, their overall health, their risk factors, and their home care routines. Properly educating our patients on what is going on in their mouths and the impact it has on the rest of their body is imperative. GBT enables us to flip the script and engage our patients to understand their own oral health. Prioritizing disclosing and education at the beginning of the dental appointment is paramount. This is the time that your patient will be most engaged in their oral health and periodontal education and recommendations will be most influential at this time. By incorporating GBT into your practice, you are able to reduce your patients bacterial load in their mouth and in turn, reduce negative systemic effects [4]. This prioritizes your patient’s overall health, all the while being efficient, effective, comfortable for the patient and ergonomic for the clinician.
Dysbiosis: what is it?
Periodontal disease affects at least 1 in 10 people, making the disease more prevalent than cardiovascular disease [3]. It is a low grade chronic inflammatory condition that is initiated by the accumulation of pathogenic bacterial biofilms[2]. This accumulation of ‘bad bacteria’ can lead to a dysbiosis in the oral cavity, which furthers the host inflammatory response, and leads to breakdown of tissue and structures that surround our teeth [5]. When our mouth is in dysbiosis, we experience a shift in the equilibrium of the good bacteria versus the bad bacteria [2]. It is imperative for our oral health and our systemic health that we promote symbiosis in our oral cavity[2]. Guided Biofilm Therapy is a new approach to preventive and non-surgical periodontal therapy that allows us to bring our oral microbiome back into balance, all while being minimally invasive, highly effective, and comfortable for the clinician and the patient[5]
What is Guided Biofilm Therapy
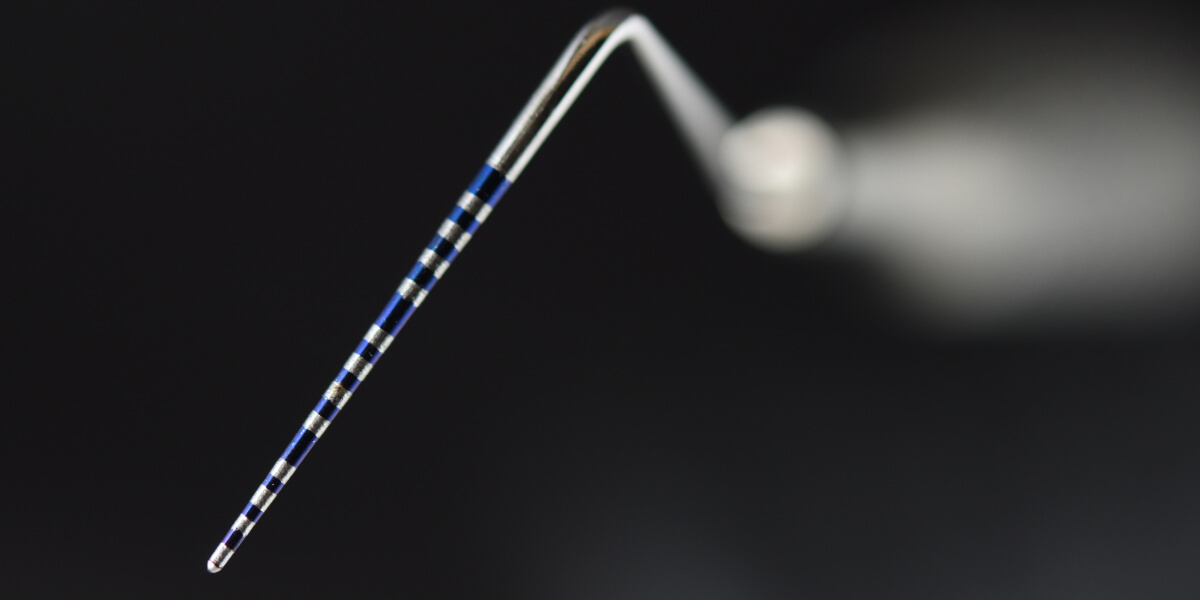
Guided Biofilm Therapy is a systematic, evidenced based approach of removing biofilm (dental plaque) in our mouths and around natural teeth and restorative materials including implants. Using the patented Airflow, Perioflow and Peizon technology in conjunction with Airflow Plus Powder and the Airflow Prophylaxis Master device, it allows for safe and effective removal of disease-causing plaque. GBT uses an 8-step compass to guide you and your patient through assessments, disclosing and complete biofilm and calculus removal. Guided Biofilm Therapy is individualized from patient to patient and is based on the patient’s diagnosis, risk assessment, and medical history[2]
It’s all in the powder!
There is one and only one authentic Airflow Plus powder. The powder technology that has engineered the Airflow Plus powder is one of the main reasons why GBT is so effective and versatile! The Plus powder is composed of erythritol, which is a food additive and a sugar substitute[1]. Erythritol is a sugar alcohol that is not metabolized by the bacteria in our mouths. This, in turn, reduces the amount of dental plaque, dental plaque acids and certain types of bacteria in our mouths that can lead to an increased risk for dental cavities[1]. Moreover, the Airflow Plus powder is safe to use on all tooth surfaces including enamel, dentin, and cementum, as well as soft tissues, restorations, implants, and dentures. You can use it on any surface in the mouth safely and effectively, as well as on any age of persons! The powder has a slightly sweet flavor that patients find mild and pleasant. We are no longer just removing biofilm and stain with our polishing techniques, but the Airflow Plus powder provides a more therapeutic effect, all the while being less invasive and more efficient than other methods of biofilm removal[5]
My Experience
Many of you may be thinking “Wow this sounds great, but how easy is it to integrate into my daily practice”? Although there are some barriers associated with incorporating GBT into your office, such as the initial investment, once you have your Airflow Prophylaxis Master device, it’s as easy as getting trained and being able to apply your knowledge and new skills the next day! The GBT training is informative and thorough to equip the clinicians with the knowledge and confidence to begin using GBT on every patient in their practice. I was nervous about changing our regular protocol in my own office. I was worried patients wouldn’t like it. I was worried about learning new skills, and what jargon to use to explain to my patients what my fancy new device was. We did however jump in feet first to Guided Biofilm Therapy and haven’t looked back! Our patients love it, the hygienists love it, and it feels so good to know that we are making a difference and a positive impact on our patient’s health!
Final Thoughts on Guided Biofilm Therapy
GBT allows dental professionals to manage dental biofilm, notably in areas that are inaccessible to our instruments and would have remained hidden otherwise[5]. Although traditional scaling and root planning has been stated to be the gold standard for periodontal therapy, studies have shown that GBT treatment is as effective in biofilm removal and debridement as scaling and root planing, yet has better patient compliance and comfort, and preserves the integrity of the teeth and the surrounding soft tissue[4]. Traditional methods of non-surgical periodontal therapy are technically demanding for clinicians and can lead to ergonomic issues and burnout. They are also more uncomfortable for our patients and can be damaging to the tooth structures[5]. GBT incorporates steps such as disclosing teeth to make biofilm visible. This allows for better education for our patients and improves patient compliance. The disclosed plaque also acts as a road map for the clinician to efficiently remove all biofilm without overtreating tooth structures or damaging soft tissues, especially sub gingivally [5]. By airflowing first, we remove all of the dental plaque, which provides better visible access to calculus deposits. This allows us to target the use of our piezon and reduce our handscaling time. This results in less patient sensitivity, minimizes soft tissue damage, reduction in treatment time and minimizes any potential clinical attachment loss (CAL) from over treating in shallow periodontal pockets [5]. Guided Biofilm Therapy is changing the way we treat our patients for their dental hygiene appointments. It incorporates education, comfort for the patient and the clinician and a scientifically proven way to bring our mouths back into symbiosis. In doing so, it reduces our risk for bacteremia and complications with the oral systemic link[2]. GBT is truly a game changer for the dental profession and will change the way we practice dental hygiene going forward. It has changed the way I look at debriding my patient’s mouths and has brought so much joy to my practice!
- de Cock P. (2018). Erythritol Functional Roles in Oral-Systemic Health. Advances in dental research, 29(1), 104–109. https://doi.org/10.1177/0022034517736499
- Herrera, D., Sanz, M., Shapira, L., Brotons, C., Chapple, I., Frese, T., Graziani, F., Hobbs, F. D. R., Huck, O., Hummers, E., Jepsen, S., Kravtchenko, O., Madianos, P., Molina, A., Ungan, M., Vilaseca, J., Windak, A., & Vinker, S. (2023). Association between periodontal diseases and cardiovascular diseases, diabetes and respiratory diseases: Consensus report of the Joint Workshop by the European Federation of Periodontology (EFP) and the European arm of the World Organization of Family Doctors (WONCA Europe). Journal of clinical periodontology, 50(6), 819–841.https://doi.org/10.1111/jcpe.13807
- Janakiram, C., & Dye, B. A. (2020). A public health approach for prevention of periodontal disease.. Periodontology 2000, 84(1), 202–214. https://doi.org/10.1111/prd.12337
- Mutthineni, Ramesh. (2022). Guided biofilm therapy (GBT) in periodontal disease and peri-implant disease. IP International Journal of Periodontology and Implantology, 7(4), 143-144. 10.18231/j.ijpi.2022.031.
- Shrivastava, D., Natoli, V., Srivastava, K. C., Alzoubi, I. A., Nagy, A. I., Hamza, M. O., Al-Johani, K., Alam, M. K., & Khurshid, Z. (2021). Novel Approach to Dental Biofilm Management through Guided Biofilm Therapy (GBT): A Review. Microorganisms, 9(9), 1966. https://doi.org/10.3390/microorganisms9091966